| What is the prostate? | ||||
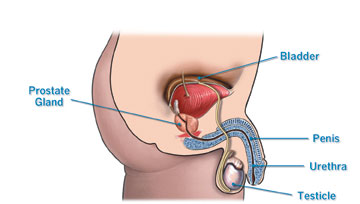
| The prostate is part of the male reproductive system, is about the same size and shape as a walnut and weighs about an ounce. It is located below the bladder and in front of the rectum, and surrounds the urethra, the tube-like structure that carries urine from the bladder out through the penis. The main function of the prostate is to produce ejaculatory fluid. | ||||
| What is BPH? | ||||
| Benign prostatic hyperplasia (BPH), formerly known as prostatism, is a common urological condition caused by the non-cancerous enlargement of the prostate gland in aging men. As the prostate enlarges, it can squeeze down on the urethra. This can cause men to have trouble urinating leading to the symptoms of BPH. | ||||
| What are some of the risk factors for BPH? | ||||
| Risk factors for developing BPH include increasing age and a family history of BPH. | ||||
| What are some of the symptoms associated with BPH? | ||||
| Since the prostate surrounds the urethra just below the bladder, its enlargement can result in symptoms that irritate or obstruct the bladder. A common symptom is the need to frequently empty the bladder, sometimes as often as every two hours or more, especially at night. Other symptoms include the sensation that the bladder is not empty, even after a man is done urinating, or that a man cannot postpone urination once the urge to urinate arises. BPH can cause a weak urinary stream, dribbling of urine, or the need to stop and start urinating several times when the bladder is emptied. BPH can cause trouble in starting to urinate, often requiring a man to push or strain in order to urinate. In extreme cases, a man might not be able to urinate at all, which is an emergency that requires prompt attention. | ||||
| How is BPH diagnosed? | ||||
In order to help assess the severity of such symptoms, the International prostate symptoms Score Index(IPSS) was developed. This diagnostic system includes a series of questions that ask how often the urinary symptoms identified above occur. This helps measure how severe the BPH is — ranging from mild to severe. When a doctor evaluates someone for possible BPH, the evaluation will typically consist of a thorough medical history, a physical examination (including a digital rectal exam or DRE), and use of the IPSS Symptom Score Index. There are a series of other studies that may or may not be offered to a patient being evaluated for BPH depending on the clinical situation. These include:
|
||||
| When should I see a doctor about BPH? | ||||
| A man should see a doctor if he has any of the symptoms mentioned previously that are bothersome. In addition, he should see a doctor immediately if he has blood in the urine, pain with urination, burning with urination or is unable to urinate. | ||||
| Is BPH a rare condition? | ||||
| No, it is very common. It will affect approximately 50 percent of men between the ages of 51 and 60 and up to 90 percent of men over the age of 80. | ||||
| Does BPH lead to prostate cancer? | ||||
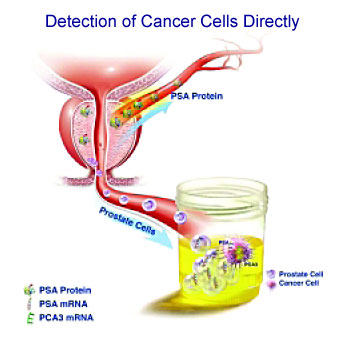
| No, BPH is not cancer and cannot lead to cancer, although both conditions can exist together. There are usually no symptoms during the early stages of prostate cancer, and so yearly physical examinations and PSA tests are highly recommended to eliminate cancer diagnosis. | ||||
| Which type of drugs are the best? | ||||
| To date, there is not enough research data to predict who will respond to medical therapy or which drug will be better for an individual patient. | ||||
| How do I know if oral medications are the best treatment for me? | ||||
| If you are diagnosed with BPH, you should discuss all treatment options with your urologist. Together, you can decide whether medication or surgical treatment is best for you | ||||
| Enlarged Prostate (BPH)? | ||||
|
||||
| Many men report changes to lifestyle such as avoiding travel, interruption of leisure activities and using bathroom stalls instead of urinals. Frequent trips to the bathroom can disrupt sleep. | ||||
| A Simple and Effective Solution | ||||
|
||||
|
||||
Words to Know
You may first notice symptoms of enlarged prostate (BPH) yourself, or your doctor may find that your prostate is enlarged during a routine checkup. When enlarged prostate (BPH) is suspected, you may be referred to a urologist, a doctor who specializes in problems of the urinary tract and the male reproductive system. Several tests help the doctor identify the problem and decide the best course of treatment. The tests vary from patient to patient, but the following are the most common. |
||||
Digital Rectal Exam (DRE)This exam is usually the first test done. The doctor inserts a gloved finger into the rectum and feels the part of the prostate next to the rectum. This exam gives the doctor a general idea of the size and condition of the gland. Prostate Specific Antigen (PSA) Blood TestIn order to rule out cancer as a cause of urinary symptoms, your doctor may recommend a PSA blood test. PSA, a protein produced by prostate cells, is frequently present at elevated levels in the blood of men who have prostate cancer. Rectal UltrasoundIf there is a suspicion of prostate cancer, your doctor may recommend a test with rectal ultrasound. In this procedure, a probe inserted in the rectum directs sound waves at the prostate. The echo patterns of the sound waves form an image of the prostate gland on a display screen. Urine Flow StudySometimes the doctor will ask a patient to urinate into a special device which measures how quickly the urine is flowing. A reduced flow often suggests BPH. Intravenous Pyelogram (IVP)IVP is an x-ray of the urinary tract. In this test, a dye is injected into a vein, and the x-ray is taken. The dye makes the urine visible on the x-ray and shows any obstruction or blockage in the urinary tract. CystoscopyIn this exam, the doctor inserts a small tube through the opening of the urethra in the penis. This test allows the doctor to determine the size of the gland and identify the location and degree of the obstruction. |
||||
| Understanding enlarged prostate | ||||
| When men reach their mid-50’s, their chances of experiencing bothersome urinary symptoms increase. In many cases, a physician will find that an enlarged prostate is the cause. As the prostate gland naturally grows, it can compress the urethra—the tube that drains urine from the body. This results in enlarged prostate symptoms. To learn more about an enlarged prostate (also called Benign Prostatic Hyperplasia or BPH), | ||||
| Treating enlarged prostate—and getting back to what matters most | ||||
| An enlarged prostate not only interferes with your health, it can disrupt your lifestyle and put a strain on the relationships you value most. If urinary issues are interfering with your daily activities, it’s time to explore your options.
No solution is right for everyone. Some choose to manage their enlarged prostate symptoms—others decide to permanently treat the condition and restore their prostate health. Understand what BPH treatments are available and discuss them with your doctor to find the solution that’s right for you. |
||||
| What are my BPH treatment options? | ||||
| Based on your enlarged prostate symptoms and your desired outcome, your doctor can recommend a number of BPH treatment options:
Watchful Waiting – In cases when enlarged prostate symptoms are mild, doctors may recommend a “watch and wait” approach, often asking patients to track BPH symptoms, before pursuing other courses of treatment. Enlarged Prostate Medications – Physicians will often prescribe medications to manage enlarged prostate symptoms. These medications include alpha blockers, which relax the muscles around the neck of the bladder, making it easier to urinate, and alpha reductase inhibitors, drugs intended to shrink the prostate gland. Microwave and Heat Therapies – These are minimally invasive treatments that use microwave or heat energy to reduce the symptoms of an enlarged prostate. Transurethral Resection of the Prostate (TURP) – This is a surgical procedure to remove enlarged prostate tissue. Laser Therapy – This option removes enlarged prostate tissue through the use of high energy lasers. Prostatic Stents – This option is reserved for those patients who are severely obstructed and otherwise unable to undergo surgery. Enlarged Prostate Treatments: Knowing the Advantages and Disadvantages Transurethral Microwave Thermotherapy of the Prostate (TUMT) TherMatrx Safe and effective office-based solution Watchful Waiting Symptoms may improve 2 Surgery Transurethral Resection of the Prostate (TURP) Provides long-lasting symptom relief Medications Alpha Blockers (Relax muscles around the bladder neck making it easier to urinate.) 2 AUA Symptom Score is lowered by 6 to 8 points 1 5 Alpha-reductase Inhibitors (Helps shrink the prostate) 2 AUA Symtom Score is lowered by 3 to 4 points 1 |